
Almost all of the patients that come to our office complaining of heel pain think that they have a heel spur. Some do, some don’t but almost ALL of them are not having pain from the heel spur itself.
We know that a heel spur is a bony projection from the large bone of our heel called the calcaneous. Bone does not have any nerve endings so it can’t cause a lot of pain. Most pain in our heel is from damage or inflammation of the soft tissue of the heel. This is called the plantar fascia.
Not all heel pain is treated the same. Getting the right diagnosis is essential for proper treatment. Once we determine the exact cause of the heel pain, we can start the proper treatment plan to help reduce the pain. Not diagnosing the cause properly and starting the wrong treatment can sometimes make the heel condition more painful. This is not always that easy. There are many health providers who do not understand the different causes of heel pain and start the wrong treatment making the condition worse.
We believe there are four major problems with our heels that cause ninety percent of all heel pain. Each one has either a different location or onset of pain. By determining the exact location of the pain and when in the day the pain is the worst, we can usually diagnose the problem with a high level of accuracy.
The four major problems that can affect the heel are plantar fasciitis of the non weight bearing area of the plantar fascia, plantar fasciitis of the weightbearing area of the plantar fascia, retrocalcaneal bursitis and heel neuritis. It is very important to note that there are other etiologies that can cause heel pain. These include but are not limited to rheumatoid arthritis, gout, psoriasis, fractures of the heel, growth plate abnormalities in children and bone tumors. It is essential to note that if your heel pain does not get better and seems to be getting worse; these other problems must be ruled out.
very treatment plan has the ultimate goal of reducing the patient’s pain. We treat heel pain on three different levels in the office. We use injectable medication for three weeks, oral medication for four weeks but the secret to help make these medications work is to control the forces that made the heel hurt in the first place. If you do not control these forces then no other treatment plans including medication, injection, stretching exercises or physical therapy will be 100% effective. This means putting something in the shoe that will control each of the four major problems that can affect the heel.
We will talk about each of the four problems, how we treat them in the office and what you can do a home.

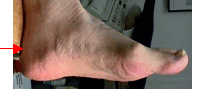
Plantar fasciitis is the most common heel pain syndrome that we see in our office. It is also the easiest to treat and has the highest success rate. Ninety percent of all people with this condition get better with conservative care. The plantar fascia is a thick ligament that runs from the heel bone to the toes. It is a major supporter of the arch. Anything that puts increased pressure on the arch can start this condition. The pain is located on the inside of our foot right at the edge of where we start to feel our heel bone. The first step in the morning is the worst. After a few steps it seems to get better. The pain returns after we sit back down for a short time and go to stand back up again.
Conservative treatment renders ninety percent of all patients pain free. In our office on a first visit we usually take x-rays to rule out any other problems. We recommend a combined treatment of a series of three injections of a cortisone type medication at weekly intervals to treat the acute inflammation. We recommend a non-steroidal oral medication to be taken concurrently for four to five weeks. This treats the chronic inflammation. The secret to this condition is to control the arch. We control the arch and the plantar fascia by taping the foot so as to not let it stretch out. For long term control we place an orthotic(arch support) in the shoe. This can be an over the counter or a more custom fitted arch support.
At home you can try a couple of simple things. After any prolonged walking or being on your feet all day you should ice the bottom of your foot. This helps decrease the amount of inflammation. Take aspirin, not Tylenol, two pills twice a day for four weeks. You can also try Motrin or Aleve. If this upsets your stomach stop taking the medication. Try an over the counter arch support to control some of the stretching of the plantar fascia. A gym shoe especially a high top one will control not only the plantar fascia but also heel motion and the amount of shock the heel gets in normal walking.
Since 90% of all patients get better with conservative care, it rarely requires surgical intervention. The surgery consists of releasing the plantar fascia from the calcaneous. This can be accomplished by a very small incision on the inside of the heel. A new treatment modality is now available. Extracorporeal shock wave therapy uses a machine similar to the one used for kidney and gallstones. This machine is indicate only for chronic proximal plantar fascitis.

Plantar fasciitis of the weightbearing area of the plantar fascia is a condition where the normal padding under the heel is defective. As we walk we traumatize our heel. Many of our modern shoes have no cushioning under the heel especially a woman’s flats. The plantar fascia gets injured and inflamed right under the heel. The symptoms are exactly the same as with plantar fascitis. There is morning pain when you first get out of bed and pain after you sit for a while and get back up. The only difference is the location of where the pain is. Instead of on the inside of the arch area the pain is directly under the heel.
Conservative care helps about seventy-five percent of our patients with their pain. On the first visit to our office we take x-rays to rule out any other problems. We recommend a series of three injections of a low dose medication into the bursal sack. Again we use an oral non-steroidal medication for four to five weeks duration. The secret to this condition is to control heel strike. Instead of controlling the arch we want to protect the heel from further trauma. We recommend a heel cup of a soft material, usually a viscoelastic compound with a very soft center. We have designed an orthotic that has alot of padding right under the heel.
At home you can again apply ice after any exercise or prolonged walking. Take aspirin, Motrin or Aleve as directed. Protecting your heel is essential. This is done by wearing shoes with soft insoles and putting something soft in your shoes. Going barefoot around the house makes this condition worse.
Surgery on this condition is very similar to that of non weight bearing plantar fascia.
This is the only condition we will talk about that affects the back of the heel. Where the Achilles tendon attaches to the heel bone is the site of this condition. The pain is similar to plantar fasciitis and heel bursitis in that the morning is the time the pain is the worst. After we sit and stand back up it can hurt again. There is usually a prominence of bone we can feel in the back of our heel. This condition affects women to a greater extent because of the type of shoes they wear.
Conservative care helps only seventy percent of our patients. On a first visit to the office we take special x-rays of the heel. We recommend a stretching program to our patients to try to reduce the inflammation and stretch out the Achilles tendon. We do not give any injections of steroid to the back of our heels. This can weaken the Achilles tendon causing it to detach. Our treatment plan consists of a stretching program and oral anti-inflammatory medication for four weeks. There is a new form of physical therapy we have been using that has been very helpful in reducing the pain. This is called acetic acid iontophoresis. It is more successful when used early on in the treatment process. The secret to this condition is to control heel strike, heel motion in the back of the shoe and physically protect the back of the heel from the shoe. This is done by using a Tuli’s heel cup. The Tuli's heel cup protects the back of the heel from irritation by the shoe. If this does not give enough relief then a custom orthotic with a deep heel cup is recommended.
At home you can try a few things. Using a high top gym shoe protects the back of our heel and controls heel motion. Again try aspirin, Motrin or Aleve as directed if you can take tolerate the medication. Ice your Achilles tendon after exercise. Start a stretching program to the back of your leg. Start using a Tuli’s heel cup immediately.
The surgeries for this condition are pretty successful. They require removing the bone spurs from the back of the heel and possibly remodeling the heel bone. The Achilles tendon attaches to the bone in the back of the heel. If too much of the Achilles has to be removed from the bone it has to be reattached with metal anchors. The recovery period form this procedure can be up to 6-8 weeks.
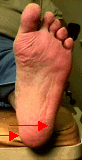
This is the only condition with nerve involvement. This is the most commonly misdiagnosed condition of the heel. Since we treat a lot of heels we see more of this condition than any other. The reason that this number is so high is that with any of the other conditions most patients respond to the conservative treatment plans. If heel neuritis is misdiagnosed as plantar fascitis and a rigid type arch support is used the condition will get worse. Getting the proper diagnosis is essential. Only forty percent of patients with this condition get pain free. This is the worst condition of the heel to have and it is the most painful. Although there still might be some morning pain and pain when rising the hallmark of this condition is that the pain never goes away and progressively gets worse as the day goes on. The pain is very sharp and at times can cause intense burning. Sometimes there is a sharp shooting pain that travels up the leg. The pain is far more severe than any of the other conditions of the heel. Many patients have so much pain as they walk that they transfer the weight from their heel to their toes. This can cause increased pain in the ball of the foot and make the Achilles tendon behind the heel very sore. There are two different nerve roots that can be involved. The first is on the inside of the foot. The other, which is more severe, is on the bottom and outside of the foot.
Conservative care helps only sixty percent of patients get pain free. On the first visit we review x-rays, recommend a treatment of a series of three injections of a steroid type compound and oral anti-inflammatory medication for four weeks. The secret to this condition is again to control heel strike. We again recommend a UCO heel cup. This heel cup works by controlling the shock of the heel hitting the ground. If this does not give enough relief of the pain then we recommend our newly designed orthotic that not only controls heel strike but the shearing forces of the heel as in inverts and everts during walking. We have had great success with this device.
At home you treat this condition the same as heel bursitis. Apply ice after any exercise or prolonged walking. Take aspirin, Motrin or Aleve as directed. Protecting your heel with a UCO heel cup is essential in this condition. Anything that can injure your heel must be avoided especially going barefoot.
Surgery for these two conditions are a little more technical. The medial calcaneal nerve is a sensory nerve only. It has no motor function. If the pain becomes unbearable then you can stop the pain by stopping the nerve from functioning. This is done by either chemical neurolysis with alcohol or possible surgical transection. The first branch of the lateral plantar nerve is another story. It has a motor function in the foot so chemical neuroysis or transection is not recommended. Open reduction is required. This is only 60% successful.
This is where it can get a little confusing. Many patients don’t present with just one of the four heel syndromes. Many times they will present with two and even three of the conditions at the same time. Usually weight bearing and non weight bearing plantar fasciitis and heel bursitis will be in combination. Most of the time retrocalcaneal bursitis is not in combination with the other heel syndromes. So sometimes there is morning pain, which eases off a little after walking, but there is increased pain as the day goes on. It is important to treat the condition with the worst prognosis first. We will treat heel neuritis as the primary complaint followed by plantar fasciitis of the weight bearing area and then plantar fasciitis of the non weight bearing area. Heel neuritis and plantar fasciitis of the weight bearing area can pretty much be treated the same.
The problem comes in when you have plantar facial pain with either or both heel neuritis and . You treat the neuritis or plantar fasciitis of the weight bearing area as the primary complaint. Using the gel heel cups and taking aspirin will help both the neuritis and the plantar fasciitis of the weight bearing area pain. When you use the gel heel cup it raises your heel up a little and that stretches out the plantar fascia potentially causing the non weight bearing plantar fasciitis to get worse. If you use a regular orthotic that is hard on the top, the non weight bearing plantar facial pain will go away but the heel neuritis and plantar fsaciitis of the weight bearing area will become unbearable. If after you try the gel heel cup are still having increased weight bearing plantar facial pain you might be a candidate for our newly designed custom orthotic, which controls the plantar fascia and cushions the heel. This orthotic is the only thing we use to treat combination heel syndromes involving the plantar fascia. This orthotic has greatly improved our success rate with combination heel syndromes.
Phone: